Evaluation and Management of the Infant Exposed to HIV-1 in the United States
- 2004 recommendations: Start trimethoprim-sulfamethoxazole starting at 4-6 weeks of age, because excluding HIV required tests at 1 month and another test at 4 months. Both tests had to be negative before stopping Bactrim. Dx was made by HIV DNA PCR.
- 2009 recommendations: When tests at 2 and 4 weeks are negative, infants do not need any treatment with trimethoprim-sulfamethoxazole. Diagnosis can be made by HIV DNA PCR or RNA PCR testing.Despite 600 HIV-infected women giving birth every year, there are fewer than 200 babies born with HIV infection. See below:
Summary
· Whenever possible, maternal HIV-1 infection should be identified before or during pregnancy, which allows earlier initiation of care for the mother and for more effective interventions to prevent MTCT. The AAP recommends documented, routine HIV-1 antibody testing for all pregnant women in the United States, after notifying the patient that testing will be performed, unless the patient declines HIV-1 testing ("opt-out" consent, or "right of refusal"). All HIV-1 antibody testing should be performed in a manner consistent with state and local laws. In states where laws and regulations require written informed maternal consent for testing, practitioners should work to modify the laws or regulations to permit opt-out consent.
· If the mother's HIV-1 serostatus is unknown at the time of labor or birth, the newborn infant's health care provider should perform rapid HIV-1 antibody testing on the mother or the newborn infant with appropriate consent consistent with state and local laws. The results should be reported to health care providers quickly enough to allow effective ARV prophylaxis to be administered to the infant as soon as possible after birth but certainly by 12 hours after birth.
· ARV prophylaxis for the mother and newborn infant should be administered promptly on the basis of a positive rapid antibody test result without waiting for results of confirmatory HIV-1 testing, and breastfeeding should not be initiated. If the rapid test result is positive, confirmatory testing should be performed, and if confirmatory test results are negative (indicating that the infant was not truly exposed to HIV-1), then ARV prophylaxis should be stopped and breastfeeding can be initiated.
· In the United States, HIV-1–infected mothers should not breastfeed their infants and should be educated about safe alternatives.
· Maternal health information should be reviewed to determine if the infant may have been exposed to maternal coinfections such as TB, syphilis, toxoplasmosis, hepatitis B or C, cytomegalovirus, or herpes simplex virus. Diagnostic testing and treatment of coinfections in the infant are based on maternal findings and evaluation of the infant.37
· Pediatricians should provide counseling to parents and caregivers of HIV-1–exposed infants about HIV-1 infection, including anticipatory guidance on the course of illness, infection-control measures, care of the infant, diagnostic tests, and potential drug toxicities.
· All HIV-1–exposed infants should undergo virologic testing with HIV-1 DNA or RNA assays at 14 to 21 days of age, and if results are negative, tests should be repeated at 1 to 2 and 4 to 6 months of age to identify or exclude HIV-1 infection as early as possible. For children with negative virologic test results, many experts confirm the absence of HIV-1 infection with HIV-1 antibody assay testing at 12 to 18 months of age. If any test result is positive, the test should be repeated immediately for confirmation.
· Initial testing in the first few days of life allows identification of in utero infection and might be considered if maternal ARVs were not administered during pregnancy or in other high-risk situations. If HIV-1 RNA or DNA testing of the newborn infant was not performed shortly after birth, or if such test results were negative, diagnostic testing with HIV-1 NAAT is delayed until 14 to 21 days of age, because the diagnostic sensitivity of virologic assays increases rapidly by 2 weeks of age.
· For nonbreastfeeding infants and children younger than 18 months with no positive HIV-1 virologic test results, presumptive exclusion of HIV-1 infection is based on 2 negative HIV-1 RNA or DNA virologic test results from separate specimens, both of which were obtained at  2 weeks of age and 1 of which was obtained at
2 weeks of age and 1 of which was obtained at  4 weeks of age; 1 negative HIV-1 RNA or DNA virologic test result obtained at
4 weeks of age; 1 negative HIV-1 RNA or DNA virologic test result obtained at  8 weeks of age; or 1 negative HIV-1 antibody test result obtained at
8 weeks of age; or 1 negative HIV-1 antibody test result obtained at  6 months of age. If these test results are negative, further testing is required to definitively exclude HIV-1 infection.
6 months of age. If these test results are negative, further testing is required to definitively exclude HIV-1 infection.
· For nonbreastfeeding infants and children younger than 18 months of age with no positive HIV-1 virologic test results, definitive exclusion of HIV-1 infection is based on 2 negative HIV-1 RNA or DNA virologic test results from separate specimens, both of which were obtained at  1 month of age and 1 of which was obtained at
1 month of age and 1 of which was obtained at  4 months of age, or 2 negative HIV-1 antibody test results from separate specimens, both of which were obtained at
4 months of age, or 2 negative HIV-1 antibody test results from separate specimens, both of which were obtained at  6 months of age. Further testing is suggested to confirm the absence of HIV-1 infection.
6 months of age. Further testing is suggested to confirm the absence of HIV-1 infection.
· Many experts confirm the absence of HIV-1 infection with a negative HIV-1 antibody assay result at 12 to 18 months of age. These laboratory tests can only be used to exclude HIV-1 infection if there is no other laboratory or clinical evidence of HIV-1 infection (ie, no subsequent positive results from virologic tests if tests were performed and no AIDS-defining condition for which there is no other underlying condition of immunosuppression).
· For breastfeeding infants, a similar testing algorithm can be followed, with timing of testing based on the date of complete cessation of breastfeeding instead of the date of birth.
· Infants born of HIV-1–infected mothers should be considered for PCP prophylaxis beginning at 4 to 6 weeks of age. Infants with indeterminate HIV-1 infection status should receive prophylaxis until they are determined presumptively or definitively not to be infected with HIV-1. Prophylaxis is not recommended for infants who meet criteria for presumptively or definitively not infected with HIV-1 (see "Interpretation of Negative HIV-1 Test Results").
· All infants exposed to ARV agents in utero or as infants should be monitored for short- and long-term drug toxicity.
· Immunizations and TB screening should be provided for HIV-1–exposed infants in accordance with published guidelines.37
· HIV-1 testing should be offered and recommended to family members of HIV-1–exposed infants.
· The practitioner providing care for the HIV-1–exposed or HIV-1–infected infant should consult with a pediatric HIV-1 specialist. If the HIV-1–infected mother is an adolescent, consultation with a practitioner familiar with the care of adolescents is advised.
2009 Management of Infants Exposed to HIV
Evaluation and Management of the Infant Exposed to HIV-1 in the United States. Peter L. Havens, MD, Lynne M. Mofenson, MD and the Committee on Pediatric AIDS. PEDIATRICS Vol. 123 No. 1 January 2009, pp. 175-187 (doi:10.1542/peds.2008-3076)
Full text:
The pediatrician plays a key role in the prevention of mother-to-child transmission of HIV-1 infection. For infants born to women with HIV-1 infection identified during pregnancy, the pediatrician ensures that antiretroviral prophylaxis is provided to the infant to decrease the risk of acquiring HIV-1 infection and promotes avoidance of postnatal HIV-1 transmission by advising HIV-1–infected women not to breastfeed. The pediatrician should perform HIV-1 antibody testing for infants born to women whose HIV-1 infection status was not determined during pregnancy or labor. For HIV-1–exposed infants, the pediatrician monitors the infant for early determination of HIV-1 infection status and for possible short- and long-term toxicity from antiretroviral exposures. Provision of chemoprophylaxis for Pneumocystis jiroveci pneumonia and support of families living with HIV-1 by providing counseling to parents or caregivers are also important components of care.
Key Words: human immunodeficiency virus • HIV-1 • perinatal transmission • antiretroviral prophylaxis • diagnosis • infant
Abbreviations: MTCT—mother-to-child transmission • ARV—antiretroviral • AAP—American Academy of Pediatrics • PCP—Pneumocystis jiroveci pneumonia • CDC—Centers for Disease Control and Prevention • ZDV—zidovudine • TB—tuberculosis • NAAT—nucleic acid amplification test • PCR—polymerase chain reaction • BCG—bacille Calmette-Guérin • TST—tuberculin skin test
Introduction
Each year in the United States, approximately 6000 pregnant women infected with HIV-1 give birth. Implementation of effective, cost-saving1–3 preventive strategies during pregnancy has reduced the risk of mother-to-child transmission (MTCT) of HIV-1 to approximately 1% to 2%.4 Preventive strategies include universal HIV-1 antibody testing of all pregnant women and, for women who are infected with HIV-1, (1) administration of antiretroviral (ARV) prophylaxis during pregnancy and labor and to the infant for 6 weeks after birth; (2) elective cesarean delivery before the onset of labor and before rupture of membranes for women with an HIV-1 viral load of >1000 copies per mL before delivery; and (3) complete avoidance of breastfeeding.5,6 These strategies have been outlined in a separate American Academy of Pediatrics (AAP) policy statement titled "HIV Testing and Prophylaxis to Prevent Mother-to-Child Transmission in the United States."7 The current clinical report offers companion guidance on the evaluation and management of the HIV-1–exposed infant after birth.
The pediatrician plays a key role in prevention of MTCT of HIV-1 by (1) identifying HIV-1–exposed infants even if the mother's HIV-1 infection was not recognized before delivery; (2) prescribing ARV prophylaxis for infants born to HIV-1–infected women to reduce the risk of MTCT of HIV-1; and (3) further reducing the risk of HIV-1 transmission by advising women with HIV-1 infection not to breastfeed. In addition to standard pediatric care, the pediatrician is also responsible for (1) monitoring of the infant for early determination of HIV-1 infection status, (2) evaluation for possible short- and long-term toxicities of in utero and neonatal ARV exposure, (3) providing chemoprophylaxis for Pneumocystis jiroveci pneumonia (PCP) as required, (4) administering vaccines as appropriate, and (5) supporting families living with HIV-1 infection, including providing counseling to parents or caregivers. Care of the infant or child with perinatal infection with HIV-1 should be undertaken in consultation with a pediatric HIV specialist.
Continuing technologic and medical advances in the prevention, diagnosis, and treatment of pediatric HIV-1 infection require an ongoing assessment and review of recommendations relating to management of infants known to be exposed to HIV-1 infection. This report updates previous AAP guidelines.8
Identification of Maternal HIV Infection
Although there has been a dramatic decline in the number of new HIV-1 infections in infants in the United States since 1994, when ARV prophylaxis was first documented to prevent MTCT,9 transmission continues to occur.4 Many of these infant infections could have been prevented if HIV-1 infection had been identified in their mothers through adequate preconception and prenatal care and if appropriate prophylactic interventions had been performed. The Centers for Disease Control and Prevention (CDC), the AAP, and the American College of Obstetricians and Gynecologists recommend documented, routine HIV-1 antibody testing for all pregnant women in the United States after notifying the patient that testing will be performed, unless the patient declines HIV-1 testing ("opt-out" consent or "right of refusal"5,7,10). All HIV-1 antibody testing should be performed in a manner consistent with state and local laws. (A compendium of state HIV testing laws can be found at www.nccc.ucsf.edu/StateLaws/Index.html.)
Identification of HIV-1 infection early in pregnancy affords the greatest ability to treat the pregnant woman for her HIV-1 infection for her own health and to prevent MTCT of HIV-1. Rapid HIV-1 antibody testing allows timely identification of HIV-1 infection in women even late in pregnancy, during labor, or in the immediate postpartum period as well as rapid identification of the exposed infant whose mother's HIV-1 status is unknown. The results can be available quickly enough to allow successful ARV interventions, which can reduce MTCT of HIV-1, when administered to the mother late in pregnancy or during labor or even to the infant when administered within the first few hours of life. Rapid HIV-1 antibody testing should be immediately available at all facilities with maternity services and/or a neonatal care unit.
HIV-1 Testing of the Infant if the Mother's HIV-1 Infection Status Is Unknown
For newborn infants whose mother's HIV-1 serostatus is unknown, the newborn infant's health care provider should perform rapid HIV-1 antibody testing on the mother or the infant with appropriate consent as required by state and local law. Test results should be reported to health care providers quickly enough to allow effective ARV prophylaxis to be administered to the infant as soon after birth as possible but certainly within 12 hours of life.5,7,11,12 ARV prophylaxis for mother and newborn infant to prevent MTCT of HIV-1 should be administered promptly solely on the basis of a positive rapid antibody test result, without waiting for results of confirmatory HIV-1 testing. Initiation of breastfeeding should be postponed while awaiting results of confirmatory testing. If confirmatory test results are negative, then prophylaxis should be stopped and breastfeeding may be initiated.
Interventions for Prevention of Peri-natal HIV Transmission
Maternal ARV Prophylaxis to Prevent Perinatal HIV-1 Transmission
Prenatal ARV Prophylaxis
In the United States, most pregnant women with HIV-1 infection receive care during the prenatal period, which allows (1) institution of effective ARV prophylaxis for the prevention of MTCT and ARV treatment if required for maternal health, (2) decisions to be made regarding optimal mode of delivery, and (3) counseling to the mother not to breastfeed. Current US Public Health Service guidelines for prevention of MTCT recommend use of combination ARV regimens including at least 3 ARV drugs during pregnancy and labor for all pregnant women with HIV-1 infection. ARV agents are discontinued for the mother after birth unless such therapy is required for her own health, in which case ARV therapy is continued by following guidelines for nonpregnant HIV-1–infected adults. For women who are not being treated with ARV drugs and who have very low viral load (<1000 copies per mL), some experts would consider use of zidovudine (ZDV) alone during pregnancy for prophylaxis of MTCT, stopping the drug after birth.6,13
Interventions During Labor and at Delivery
Intravenous ZDV should be administered to all pregnant women with HIV-1 infection during labor even if they receive combination ARV therapy during pregnancy and viral load is undetectable, unless there is a contraindication to maternal receipt of ZDV. Intravenous ZDV is started after the onset of labor or rupture of membranes, or approximately 3 hours before an elective cesarean delivery. There is no maximum time for use of intravenous ZDV for women with prolonged labor. Intravenous ZDV is administered at 2 mg/kg over the first hour and then continued at 1 mg/kg per hour until delivery is complete and the cord is clamped.
Elective cesarean delivery at 38 weeks' gestation is recommended for all HIV-1–infected pregnant women with HIV-1 RNA levels of >1000 copies per mL near the time of delivery (or who have unknown viral load), irrespective of maternal prenatal ARV prophylaxis.6
For women who have HIV-1 infection first identified at the time of labor, prompt initiation of maternal intrapartum prophylaxis with intravenous ZDV, followed by infant prophylaxis with ZDV for 6 weeks, is recommended, because such treatment is associated with an approximately 60% lower risk of MTCT of HIV-1 compared with no prophylaxis.6,11,12,14 In this setting, some experts may administer other ARV agents, in addition to ZDV, to both the woman during labor and the newborn infant. A detailed discussion of prophylaxis when the mother has not received antepartum ARV prophylaxis is provided in the US Public Health Service guidelines for prevention of MTCT.6
Infant ARV Prophylaxis
All HIV-1–exposed infants should receive postpartum ARV drugs to reduce the risk of perinatal HIV-1 transmission. The 6-week neonatal ZDV chemoprophylaxis regimen is recommended for all HIV-1–exposed infants,6 and a quantity of drug sufficient to finish the full course of prophylaxis should be supplied to the family before hospital discharge. Insurance providers should provide payment for this medication, and issues of availability of payment should not prevent appropriate administration of ARV agents.
In certain situations, some experts combine the 6-week infant ZDV prophylaxis regimen (Table 1) 15,16 with additional ARV drugs. Such circumstances may include those under which infants are born to mothers (1) who received prenatal ARV drugs but had suboptimal viral suppression at delivery, (2) who have received only intrapartum ARV drugs, (3) who have received no antepartum or intrapartum ARV drugs, and (4) with known drug-resistant virus. Combining the 6-week infant ZDV with other ARV drugs may provide additional efficacy for prevention of MTCT of HIV-1, but this remains unproven in clinical trials. In addition, appropriate formulations are not available for all ARV drugs, dosing regimens for neonates are incompletely defined for many drugs, and there are minimal data about the safety of combination ARV drugs in the neonate. Combination infant ARV prophylaxis, therefore, involves balancing possible benefits of enhanced prevention of MTCT of HIV-1 against risks of toxicity to the infant.
TABLE 1 Newborn Infant ZDV Dose for Prophylaxis of MTCT of HIV-115,16
Gestational Age at Birth |
Oral Dose, mg/kg per Dose |
Intravenous Dose, mg/kg per Dose |
Dosing Frequency |
Duration, wk |
|
 35 wk 35 wk
|
2 |
1.5 |
Every 6 h (a) |
6 |
>30 wk but <35 wk |
2 |
1.5 |
Every 12 h, advancing to every 8 h at 2 wk of age |
6 |
<30 wk |
2 |
1.5 |
Every 12 h, advancing to every 8 h at 4 wk of age |
6 |
|
(a) Although there are no definitive data in infants to show pharmacokinetic equivalence or equal therapeutic efficacy of administration of double the standard oral ZDV dose twice daily, for term infants administration of ZDV 4 mg/kg per dose twice daily instead of 2 mg/kg per dose every 6 hours may increase adherence to the regimen and could be considered when there are concerns about adherence to drug administration to the infant.26,77,78
The most information about use of ARV combinations in neonates is available for ZDV in combination with single-dose nevirapine17–22 and the dual combination of ZDV and lamivudine,23–27 which has been combined with daily nevirapine (although there are no published data on this last approach). Careful infant monitoring is needed if combination drugs are provided, because there may be enhanced hematologic toxicity from the combination of ZDV and lamivudine compared with ZDV alone. Long-lasting resistance is possible if the infant is already infected when prophylaxis is given, especially if nevirapine is used.28 The US Public Health Service guidelines for prevention of MTCT of HIV-1 include an extensive discussion of considerations for infant ARV prophylaxis regimens for different clinical scenarios and should be reviewed for specific recommendations.6 If drugs in addition to ZDV are considered, neonatal dosing recommendations can be found in the Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection.16 Decisions should be made in consultation with a pediatrician experienced in the care of infants and children with HIV-1 infection.
The administration of ZDV (possibly with other ARV agents) to the infant should be initiated as soon as possible after birth but certainly within 12 hours after delivery.5,7,11,12 If the infant's HIV exposure is recognized between 12 and 48 hours after delivery, ZDV prophylaxis should be initiated in that time period. Initiation of postexposure prophylaxis after 2 days of age is not likely to be efficacious in preventing transmission. Data from animal studies indicate that the longer the delay in institution of prophylaxis, the less likely that infection will be prevented. In most animal studies, ARV prophylaxis initiated 24 to 36 hours after exposure usually is not effective for preventing infection.29–31 HIV-1 infection is established in most perinatally infected infants by 1 to 2 weeks of age.32
The full 6-week course of infant ARV prophylaxis and careful instructions for its administration should be provided to the family before discharge from the hospital. A prescription and recommendations to purchase ZDV for the infant are not adequate to ensure appropriate prophylaxis. In some states, infants may not be registered for insurance for a few weeks after birth, so even if the family has insurance, coverage may not immediately be available to pay for health care costs of the infant. Some families have health insurance that covers inpatient costs but not prescription medications. Outpatient pharmacies may not stock the infant dosage form of ZDV. At hospital discharge, the family should be supplied with the medication itself, not just a prescription. Special hospital programs to support this may need to be established.
Avoidance of HIV-1 Infection From Human Milk
Postnatal transmission of HIV-1 through ingestion of human milk from a mother with HIV-1 infection is well documented, with rates as high as 9% to 15% with prolonged breastfeeding.33 In the United States, where the risk of infant mortality from infectious diseases and malnutrition is low and effective alternative sources of feeding are readily available, women with HIV-1 infection, including those receiving ARV therapy, should be counseled not to breastfeed their infants or donate their milk. Although maternal ARV therapy has been shown to reduce the concentration of cell-free HIV-1 in human milk, such therapy does not affect the amount of cell-associated virus in human milk, and there can be discordance between plasma and human milk viral load.34 It is not yet known whether maternal ARV treatment during lactation will reduce the risk of HIV-1 transmission to the infant via human milk. Ongoing studies are evaluating this question.35 In addition, there is differential penetration of ARV drugs into human milk. Some ARVs have concentrations in human milk that are much higher than concentrations in maternal plasma, and others have human milk concentrations that are much lower than in plasma or are not detectable.6,36 This raises concerns about infant drug toxicity and the potential for selection of drug-resistant virus within human milk. Thus, in the United States, where safe alternatives to breastfeeding are available, all HIV-1–infected women should avoid breastfeeding.
Counseling the mother about the avoidance of breastfeeding should occur in a culturally sensitive manner. For some women, the prohibition to breastfeed may be one of the most emotionally painful components of their efforts to protect their newborn infant from HIV-1 infection. Other mothers, particularly those who have migrated from parts of the world in which breastfeeding is nearly universal, may feel that formula feeding their infant publicizes their HIV-1 infection to family members or friends. Pediatricians should recognize the possibility that advice to not breastfeed may not always be followed and stress the importance of compliance with this intervention to prevent MTCT of HIV-1. Support for open communication regarding feeding practices is necessary to ensure appropriate follow-up and testing of all infants. Women should be educated regarding appropriate formula feeding with a discussion of the affordability of formula, including enrollment in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) when appropriate. Assistance from social service agencies may be necessary to help with education and support compliance.
Care of the HIV-1 Exposed Infant
Evaluation for Maternal Coinfections
At the time of the initial assessment of the infant, maternal health information should be reviewed to determine if the infant has been exposed to maternal coinfections, including tuberculosis (TB), syphilis, toxoplasmosis, hepatitis B or C, cytomegalovirus, or herpes simplex virus. Although there is little information as to the relative transmission or infection rates of such pathogens in infants of mothers with HIV-1 infection, there is concern that reactivation of latent infections in immunocompromised pregnant women may cause increased risk of transmission to, and disease in, exposed newborn infants. Diagnostic testing and treatment of such coinfections in infants born to women with HIV-1 infection are based both on maternal findings and evaluation of the infant.37 In the absence of suggestive history or routine evaluation, specific laboratory testing for these pathogens is not recommended.
Testing to Determine the Infant's HIV-1 Infection Status
The early identification of HIV-1 infection in exposed infants is important to allow early initiation of ARV and adjunctive therapies and care as needed. Appropriate HIV-1 diagnostic testing for infants and children younger than 18 months differs from that for older children, adolescents, and adults. Passively transferred maternal HIV-1 antibodies may be detectable in an exposed but uninfected infant's bloodstream until 18 months of age. Therefore, routine serologic testing of HIV-1–exposed infants and children is generally only informative before the age of 18 months if the test result is negative.
Assays that directly detect HIV-1 DNA or RNA (generically referred to as HIV-1 nucleic acid amplification tests [NAATs]) represent the gold standard for diagnostic testing of infants and young children under the age of 18 months. With such testing, the diagnosis or the presumptive exclusion of HIV-1 infection can be established within the first several weeks of life among nonbreastfed infants. Although neonatal ARV use may decrease the concentration of HIV-1 RNA in infant plasma in the first 6 weeks of life,38 HIV-1 DNA test results remain positive even in individuals receiving combination ARV therapy who have undetectable plasma HIV-1 RNA. The sensitivity of both DNA and RNA testing is high,39,40 so either can be used for the diagnosis of HIV-1 infection in infancy.41 False-positive results with low-level viral copy numbers have been described by using HIV-1 RNA assays,38,42,43 reinforcing the importance of repeating any positive assay result to confirm the diagnosis of HIV-1 infection in infancy.16 False-negative results are also possible, and even infants with multiple negative HIV-1 NAAT results should be retested (perhaps by using a different test) if clinical findings suggest the presence of HIV-1 infection.
The Detection of Non–Subtype B HIV-1 and of HIV-2 by NAATs
For infants born to women known or suspected to have acquired infection with non-B subtypes of HIV-1, use of HIV-1 RNA assays may be preferable to the use of HIV-1 DNA assays for diagnostic testing. Women who acquire HIV-1 infection in North America are most commonly infected with HIV-1 subtype B.44 Women who acquire HIV-1 outside of North America are often infected with other HIV-1 subtypes. Subtypes C and D predominate in southern and eastern Africa, subtype C on the Indian subcontinent, and subtype E in much of Southeast Asia.45 Currently available HIV-1 DNA polymerase chain reaction (PCR) assays may be less sensitive in the detection of non-B subtype HIV-1, and false-negative HIV-1 DNA PCR assay results have been reported in infants infected with non-B subtype HIV-1.46,47 Some of the currently available HIV-1 RNA assays have improved sensitivity for detection of non-B subtype HIV-1 infection, although even these assays may not detect all non-B subtypes, such as the uncommon group O HIV-1 strain. When testing infants suspected of infection with non-B subtype HIV-1, consultation with a pediatrician experienced in the care of infants and children with HIV infection is recommended.
HIV-2 is a retrovirus similar to HIV-1 and is found most commonly in western Africa. It is less virulent, with a slower rate of progression of clinical disease and lower rates of transmission from mother to child.48 If infant infection with HIV-2 is suspected, specific HIV-2 virologic testing must be requested, because virologic tests for HIV-1 will not identify HIV-2. Consultation with the CDC via the state department of health may be helpful in arranging this testing.
Timing of Diagnostic Testing in Infants With Known Perinatal Exposure to HIV-1
It is recommended that diagnostic testing with HIV-1 DNA or RNA assays be performed at 14 to 21 days of age and, if results are negative, repeated at 1 to 2 months of age and again at 4 to 6 months of age.41 Viral diagnostic testing in the first few days of life is recommended by some experts to allow for the early identification of infants with infection acquired in utero. For children with negative virologic tests, many experts confirm the absence of HIV-1 infection with HIV-1 antibody assay testing at 12 to 18 months of age (Table 2).
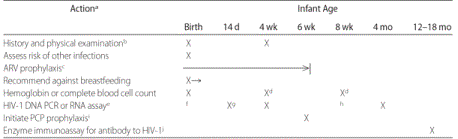
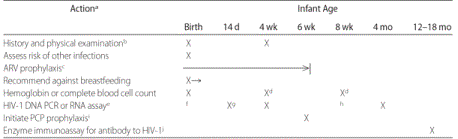
TABLE 2 Evaluation and Treatment of the Infant Exposed to HIV-1 (Birth to 18 Months of Age), in Addition to Routine Pediatric Care and Immunizations
a See text for detailed discussion of each action. If during this period the infant is diagnosed as HIV-1 infected, laboratory monitoring and immunizations should follow guidelines for treatment of pediatric HIV infection.16,37
b Review maternal health information for possible exposure to coinfections (see text). Frequency of examinations is determined, in part, by frequency of visits for immunizations in infancy.
c ARV prophylaxis is initiated as soon as possible after birth but certainly within 12 hours. ZDV prophylaxis is continued for 6 weeks, at which time it is stopped.
d Checked at 4 weeks by some experts and rechecked at 8 weeks if the week 4 hemoglobin level was significantly low.
e All HIV-1–exposed infants should undergo virologic testing for HIV-1 with HIV-1 DNA PCR or RNA assays at 14 to 21 days of age and, if results are negative, repeated at 1 to 2 and 4 to 6 months of age to identify or exclude HIV-1 infection as early as possible. Any positive test result at any age is promptly repeated to confirm the diagnosis of HIV-1 infection.
f HIV-1 DNA PCR or RNA assay testing in the first few days of life allows identification of in utero infection and might be considered if maternal ARV agents
An HIV-1 NAAT (nucleic acid amplify. test) might be considered at birth or in the first few days of life for infants at high risk of infection, including those whose mothers received no ARV drugs during pregnancy or when maternal prophylaxis was started late in pregnancy or during labor or if the mother had primary HIV-1 infection during pregnancy. In the absence of maternal ARV therapy, as many as 30% to 40% of infants with HIV-1 infection can be identified by 48 hours of age.32,49 Infants with a positive virologic test result at or before 48 hours of age are considered to have in utero infection with HIV-1, whereas infants who have a negative virologic test during the first week of life and a subsequent positive test are considered to have intrapartum infection.50 Cord blood specimens should not be used for HIV-1 RNA or DNA testing, because they are associated with an unacceptably high rate of false-positive test results.
If HIV-1 RNA or DNA testing of the newborn infant was not performed shortly after birth, or if such test results were negative, diagnostic testing with HIV-1 NAAT is delayed until 14 to 21 days of age, because the diagnostic sensitivity of virologic assays increases rapidly by 2 weeks of age. This change in assay sensitivity in the first 2 weeks of life reflects the biology of MTCT, because when HIV-1 is acquired at the time of delivery, NAAT positivity may be delayed until at or after 14 days.50 Therefore, negative results of HIV-1 DNA PCR or RNA tests performed before 14 days of age are less helpful in excluding HIV-1 infection acquired at the time of birth than are results of tests performed at or after 14 days of age.51
Management if an HIV-1 Virologic Test Result Is Positive
If any of the HIV-1 virologic test results are positive, an immediate repeat HIV-1 NAAT is recommended to confirm the diagnosis of HIV-1 infection. A diagnosis of HIV-1 infection can be made on the basis of 2 separate blood samples, each of which is positive for HIV-1 DNA or RNA. If infection is confirmed, a pediatric HIV specialist should be consulted for advice regarding ARV therapy and care. HIV-1 disease can progress very rapidly in HIV-1–infected infants, and neither CD4 T-lymphocyte count nor HIV-1 RNA copy number are reliable predictors of the risk of progression in infected infants.52 For this reason, current US pediatric HIV-1 treatment guidelines state that combination ARV treatment is recommended for all HIV-1–infected infants younger than 12 months regardless of clinical symptoms and immunologic or virologic measurements.16
Interpretation of Negative HIV-1 Test Results
On the basis of analysis of HIV-1 DNA PCR and HIV-1 RNA assay results from multiple studies, the CDC has revised the case definition for exclusion of HIV-1 infection in infants for surveillance purposes.51 The definitions supplied here are based on the CDC surveillance definitions and are appropriate for the management of children born to women with HIV-1 infection. These definitions of exclusion of HIV-1 infection are only for use in infants who do not meet the criteria for HIV-1 infection noted previously.
In nonbreastfeeding infants younger than 18 months of age with no positive HIV-1 virologic test results, presumptive exclusion of HIV-1 infection is based on:
- 2 negative HIV-1 RNA or DNA virologic test results, from separate specimens, both of which were obtained at
 2 weeks of age and 1 of which was obtained at
2 weeks of age and 1 of which was obtained at  4 weeks of age; or
4 weeks of age; or
- 1 negative HIV-1 RNA or DNA virologic test result from a specimen obtained at
 8 weeks of age; or
8 weeks of age; or
- 1 negative HIV-1 antibody test result obtained at
 6 months of age; and
6 months of age; and
- no other laboratory or clinical evidence of HIV-1 infection (ie, no subsequent positive results from virologic tests if tests were performed and no AIDS-defining condition for which there is no other underlying condition of immunosuppression).
Infants or children with these test results are presumptively not infected with HIV-1, but further testing is required to definitively exclude and then confirm the absence of HIV-1 infection. In the unusual case of an infant with a positive HIV NAAT result followed by a negative test result, an expert in care of children with HIV infection should be consulted for further testing recommendations.
In nonbreastfeeding infants with no positive HIV-1 virologic test results, definitive exclusion of HIV-1 infection is based on:
- at least 2 negative HIV-1 RNA or DNA virologic test results, from separate specimens, both of which were obtained at
 1 month of age and 1 of which was obtained at
1 month of age and 1 of which was obtained at  4 months of age, or
4 months of age, or
- at least 2 negative HIV-1 antibody test results from separate specimens obtained at
 6 months of age; and
6 months of age; and
- no other laboratory or clinical evidence of HIV-1 infection (ie, no subsequent positive results from virologic tests if tests were performed and no AIDS-defining condition for which there is no other underlying condition of immunosuppression).
Infants or children with these test results are definitively not infected with HIV-1, but follow-up testing allows confirmation of that assessment.
Many experts confirm the absence of HIV-1 infection with a negative HIV-1 antibody assay result at 12 to 18 months of age (see next section). For both presumptive and definitive exclusion of infection, the child should have no other laboratory (eg, no positive virologic test results) or clinical (eg, no AIDS-defining conditions) evidence of HIV-1 infection.
For breastfeeding infants, a similar testing algorithm can be followed, with timing of testing based on the date of complete cessation of breastfeeding instead of the date of birth.
Role of HIV-1 Antibody Testing in HIV-Exposed Infants
In HIV-1–exposed infants who are not infected with HIV-1, maternal HIV-1 antibodies transferred in utero may persist until 18 months of age (seroreversion). Many initially seropositive infants serorevert to HIV-1 antibody negativity by 12 months of age.53 Many experts confirm the absence of HIV-1 infection with a negative HIV-1 antibody assay at 12 to 18 months of age. If an HIV-1–exposed infant who is not known to be infected is tested at 12 months of age and is still antibody-positive, then testing should be repeated at 18 months of age. Performing the first antibody test at 18 months of age to confirm seroreversion may avoid the cost and pain of performing 2 tests. Loss of HIV-1 antibody in an infant with previously negative HIV-1 virologic test results definitively confirms that the infant is not infected with HIV-1. Positive HIV-1 antibodies at 18 months of age or older indicate HIV-1 infection. A positive antibody test at or beyond 18 months of age in an infant with infection previously excluded as outlined above suggests that the infant was infected after infancy, such as through breastfeeding, premastication of solid food by an HIV-1–infected caregiver,54 or sexual abuse.
Prevention of PCP
PCP is the most common serious opportunistic infection in HIV-1–infected infants and children. The highest incidence of PCP in HIV-1–infected infants is during the first year of life, with cases peaking at 3 to 6 months of age.55,56 Chemoprophylaxis is highly effective in the prevention of PCP. HIV-1–exposed infants should be considered for prophylaxis beginning at 4 to 6 weeks of age.37
Infants diagnosed with HIV-1 infection should be given prophylaxis until 1 year of age, at which time reassessment is made on the basis of age-specific CD4+ T-lymphocyte count/percentage thresholds. Trimethoprim/sulfamethoxazole is the drug of choice for prophylaxis because of its high efficacy, relative safety, low cost, and broad antimicrobial spectrum (Table 3; for further discussion see "Guidelines for the Prevention and Treatment of Opportunistic Infections Among HIV-Exposed and Infected Children"37).
TABLE 3 Regimens for PCP Prophylaxis in Infants37
Drug |
Dose |
Route |
Schedule |
|
Trimethoprim-sulfamethoxazole |
Trimethoprim 150 mg/m2 per d, with sulfamethoxazole 750 mg/m2 per d |
PO |
Twice daily for 3 d/wk on consecutive days (eg, Monday, Tuesday, and Wednesday) or on alternate days (eg, Monday, Wednesday, and Friday); alternatives: once daily for 3 d/wk or twice daily 7 d/wk |
Dapsone |
2 mg/kg |
PO |
Once daily |
|
4 mg/kg |
PO |
Once weekly |
Pentamidine |
4 mg/kg |
IV |
Every 2–4 wk |
Atovaquone |
|
|
|
Infants 1–3 mo old |
30 mg/kg |
PO |
Once daily |
Infants 4–24 mo old |
45 mg/kg |
PO |
Once daily |
|
For further discussion, see "Guidelines for the Prevention and Treatment of Opportunistic Infections Among HIV-Exposed and Infected Children."37 PO indicates per os (by mouth); IV, intravenous.
Infants with indeterminate HIV-1 infection status should receive prophylaxis starting at 4 to 6 weeks of age until they are deemed to be presumptively or definitively uninfected (see previous section). Prophylaxis is not recommended for infants who meet criteria for presumptive or definitive lack of HIV-1 infection. Thus, for infants with negative HIV-1 NAAT results at 2 and 4 weeks of age (who are presumptively not infected with HIV-1), PCP prophylaxis can be avoided altogether. If PCP prophylaxis is started at 4 to 6 weeks of age in an HIV-1–exposed infant with indeterminate HIV-1 infection status, prophylaxis can be stopped if the child subsequently meets criteria for presumptive or definitive lack of HIV infection (Table 4).
TABLE 4 Sample Clinical Scenario for Evaluation and Treatment of the Infant Exposed to HIV-1 in the United States
Timing (Infant Age) |
Action |
Comment |
|
Birth |
History and physical examination; assess risk of other infections; start ARV prophylaxis; check hemoglobin level |
HIV-1 NAATa is not needed at birth in this setting, because risk of in utero transmission is low; for infant whose mother had high virus load during pregnancy, consider HIV-1 NAAT at this time |
14 d |
HIV-1 NAAT |
If result is negative, repeat at 4 wkb,c |
4 wk |
HIV-1 NAAT |
If result is negative, HIV-1 infection is presumptively excluded (given previous negative result at  2 wk of age) 2 wk of age) |
6 wk |
Stop ARV prophylaxis |
PCP prophylaxis is not needed if HIV-1 NAAT result is negative at 14 d and 4 wk of aged |
8 wk |
No HIV-1 NAAT needed if previous test results were negative at 14 d and 4 wk of age |
A single negative result of HIV-1 NAAT performed at 8 wk of age allows presumptive exclusion of HIV-1 infectione |
4 mo |
HIV-1 NAAT |
If negative, HIV-1 infection is definitively excluded in the infant with previous presumptive exclusion |
12–18 mo |
Enzyme immunoassay for antibody to HIV |
To confirm the absence of HIV infectionf |
|
Scenario: infant born to an HIV-infected mother taking highly active ARV therapy since second trimester, virus load undetectable the week before delivery, and mother received 3 hours of ZDV intravenously before delivery.
a Either an HIV-1 DNA PCR or RNA assay.
b If any positive HIV-1 NAAT result, test is promptly repeated to confirm the diagnosis of HIV-1 infection (see "Management if an HIV-1 Virologic Test Result Is Positive").
c Some experts recommend checking hemoglobin level or complete blood cell count at 2 weeks and/or 4 weeks of age. These more frequent measurements might be warranted for preterm infants or if the baseline hemoglobin level is low.
d If no testing was performed before this or only a single test was performed between 14 days and 6 weeks of age, start PCP prophylaxis at this point until HIV infection is presumptively excluded.
e If PCP prophylaxis was started because of indeterminate HIV-1 infection status from incomplete previous testing, it can be stopped when this 8-week test result is negative.
f Many experts confirm the absence of HIV-1 infection with a negative HIV-1 antibody assay result at 12 to 18 months of age.
Prevention of TB
Although the bacille Calmette-Guérin (BCG) vaccine is routinely recommended for administration at birth to infants born in countries with a high prevalence of TB, it is not routinely administered in the United States, where TB exposure is uncommon. BCG immunization is not recommended for infants born to women with HIV-1 infection in the United States. BCG vaccine should not be administered to infants and children with known HIV-1 infection because of its potential to cause disseminated disease.37 Counseling should be provided to families originally from countries with endemic TB, because many will visit such destinations and seek BCG vaccine during those trips.
The populations at risk for infection with HIV-1 and TB overlap, and numerous studies have documented the increased risk of TB in HIV-1–infected adults. Infants and children with TB infection and disease are almost always infected by an adult in their daily environment. Therefore, information should be obtained regarding the TB infection status of the mother and other household contacts of all infants born to HIV-1–infected mothers.
HIV-1–exposed and –infected infants living in households with people who have had positive tuberculin skin test (TST) results should be evaluated for TB with a TST (5 tuberculin units of purified protein derivative) at 3 months of age and be retested at least once per year.37 Infants with a positive TST result or who have exposure to a person who has active TB (regardless of the child's TST result) should be treated for latent TB infection (after excluding active TB in the infant), according to published guidelines.37,57 If the mother or a household member has active TB that is of a contagious form (smear-positive), the infant should be separated from that person, if possible, until the person receives TB treatment and is no longer contagious (becomes smear-negative). Should the mother have documented hematogenous dissemination of TB, the infant should be evaluated for congenital TB following published guidelines.57 Consultation with a pediatric infectious disease expert should be sought.
Immunizations
Immunization schedules for children 0 to 6 and 7 to 18 years of age are published annually (www.cdc.gov/vaccines/recs/schedules/default.htm). A schedule for HIV-1–infected children is also published.37 All routine infant immunizations should be given to HIV-1–exposed infants. If HIV-1 infection is confirmed, then guidelines for the HIV-1–infected child should be followed.37 All inactivated vaccines can be administered safely to HIV-1–infected children regardless of whether the vaccine is a killed whole organism or a recombinant, subunit, toxoid, polysaccharide, or polysaccharide protein-conjugate vaccine, and the usual doses and schedules are recommended. Persons with severe cell-mediated immunodeficiency should not receive live-attenuated vaccines. However, children with HIV-1 infection are at increased risk of complications of varicella, herpes zoster, and measles compared with immunocompetent children. On the basis of limited safety, immunogenicity, and efficacy data among HIV-1–infected children, varicella and measles-mumps-rubella vaccines can be considered for HIV-1 infected children who are not severely immunosuppressed (those with CD4+ T-lymphocyte percentages of  15%).37 Note that the combined measles-mumps-rubella-varicella (MMRV) vaccine is not recommended for use in children with HIV-1. HIV-1–exposed and HIV-1–infected infants should receive 1 of the live-attenuated rotavirus vaccines at 2, 4, and 6 months of age (RotaTeq) or at 2 and 4 months of age (Rotarix). The first dose should be administered between 6 and 13 weeks of age, and the last should be administered at no later than 32 weeks of age.37
15%).37 Note that the combined measles-mumps-rubella-varicella (MMRV) vaccine is not recommended for use in children with HIV-1. HIV-1–exposed and HIV-1–infected infants should receive 1 of the live-attenuated rotavirus vaccines at 2, 4, and 6 months of age (RotaTeq) or at 2 and 4 months of age (Rotarix). The first dose should be administered between 6 and 13 weeks of age, and the last should be administered at no later than 32 weeks of age.37
Monitoring for Toxicity From in Utero and Neonatal ARV Drug Exposure
Monitoring for and Management of Short-term Toxicity During Infant ARV Prophylaxis
A baseline hemoglobin or complete blood cell and differential count should be performed on the newborn infant, because infants whose mothers have received ARV agents during pregnancy are at risk of small but measurable differences in several hematologic variables, including hemoglobin level and neutrophil and lymphocyte counts.58 The risk of anemia and neutropenia is greater in infants whose mothers were treated with combination ARV therapy during pregnancy,59,60 but anemia is also more common in infants whose mothers were treated only with ZDV compared with infants whose mothers received no ARV treatment during pregnancy.9 Nevertheless, the benefits of maternal ARV therapy in prevention of MTCT of HIV-1 clearly outweigh the risks of this hematologic toxicity in the newborn infant.61,62
Anemia is the primary clinically important complication of the 6-week ZDV regimen in the neonate, but it is unusual for the anemia to be clinically significant. Anemia associated with ZDV prophylaxis resolves when ZDV is stopped. Severe anemia that persists after prophylaxis is stopped should be further evaluated for alternative etiologies. Hematologic toxicity is more significant in infants who were exposed to antepartum ZDV in combination with other ARV drugs and in infants who received both ZDV and lamivudine as infant prophylaxis for 6 weeks.24,63 Although anemia is mild and asymptomatic in most term infants treated with ZDV, it may be more severe in preterm infants or those with additional medical problems.
Decisions about the timing of hematologic monitoring of infants treated with prophylactic ARV agents after birth depend on a number of factors, including baseline hematologic values, gestational age at birth, clinical condition of the child, receipt of concomitant medications, and maternal antepartum therapy. Some experts recheck hematologic values in a healthy infant who is receiving 6 weeks of ZDV prophylaxis only if the child is symptomatic, and others recheck hemoglobin and/or neutrophil counts after 4 weeks of ZDV treatment, particularly if the infant was born preterm or if trimethoprim/sulfamethoxazole prophylaxis is anticipated.
If hematologic abnormalities are identified, decisions on whether to continue infant ARV prophylaxis need to be individualized. Considerations include the extent of the laboratory abnormality, associated clinical symptoms, duration of infant prophylaxis already received, the magnitude of the risk of HIV-1 infection in the infant (as assessed by maternal receipt of ARV prophylaxis, maternal viral load near delivery, and mode of delivery), and availability of alternative interventions (eg, erythropoietin, red blood cell transfusion). Consultation with a pediatric HIV-1 specialist is advised if early discontinuation of prophylaxis is considered.
Routine measurement of serum lactate concentration in asymptomatic neonates to assess for potential mitochondrial toxicity is not recommended, because the clinical relevance of increased lactate concentrations is unknown, transient elevations return to normal, and predictive value for later appearance of symptomatic toxicity seems poor.64–67 However, should an infant develop severe clinical symptoms of unknown etiology, particularly neurologic symptoms, serum lactate concentration should be determined. If the serum lactate concentration is significantly abnormal in an infant with compatible clinical symptoms, an expert in pediatric HIV-1 infection should be consulted regarding potential early discontinuation of prophylaxis. In most circumstances, prophylaxis should be continued unless there is a compelling reason to stop.
Long-term Toxicity
Data remain insufficient to address the effect that exposure to ZDV or other ARV agents in utero might have on long-term risk of neoplasia or organ-system toxicities. There are conflicting data regarding whether mitochondrial dysfunction is associated with perinatal ARV exposure. Mitochondrial dysfunction should be considered in children with perinatal ARV exposure who present with severe clinical findings of unknown etiology, particularly neurologic findings.67–74
Information regarding in utero and/or neonatal ARV exposure should be part of the ongoing permanent medical chart of the child, particularly for uninfected children. Children with in utero ARV exposure who develop significant organ-system abnormalities of unknown etiology, particularly of the nervous system or heart, should be evaluated for potential mitochondrial dysfunction.71,73 Follow-up of children with ARV exposure should continue into adulthood because of the theoretical concerns regarding potential for carcinogenicity and teratogenicity of the nucleoside analog ARV drugs. Long-term follow-up should include yearly physical examinations of all children exposed to ARV drugs.
Testing Family Members
On identification of an HIV-1 exposed infant, HIV-1 screening should be recommended and offered to all immediate family members with unknown HIV-1 infection status, including the infant's father (or mother's sexual partners) and all siblings. The age of the siblings should not be a deterrent to testing, because it is possible for perinatally infected children to remain asymptomatic into adolescence.75,76
Counseling and Support
When counseling the mother of an HIV-1–exposed infant, the pediatrician should take into account that the diagnosis of HIV-1 infection may be recent for the mother, whose infection may first have been identified during or after pregnancy. The diagnosis has profound implications for the mother and the family. If the mother is not already receiving care for her HIV-1 infection, she should be referred for appropriate care for herself. Some families may require additional support because of HIV-1–associated illness or death in other family members.
Other factors that may lead to an increased need for social and psychological support services include poverty, substance abuse, depression, social isolation, lack of health care, unemployment, difficulty in finding housing, domestic violence, and fear of loss of existing supports and services, such as loss of support from a partner or loss of employment, insurance, or health care coverage. Pregnant adolescents with HIV-1 infection are a particularly vulnerable group.
For women and their families who have emigrated from other countries, there are frequently additional factors related to culture and concerns about immigration status. Many will have experienced or know of stigmatization and discrimination against people with HIV-1 infection and may have known individuals who died because they did not have access to appropriate ARV therapy. They may not have had experiences with the type of medical care available to them in the United States, which may lead to distrust or misunderstanding, complicating care and follow-up of the infant.
When counseling new parents or caregivers of an HIV-1–exposed infant, the pediatrician should provide an outline of plans for medical care for the infant. Important topics to cover include medications to prevent MTCT of HIV-1 and opportunistic infections, such as PCP, as well as the schedule of follow-up visits for assessment and laboratory assays (both for diagnosis of HIV-1 infection and to check for any adverse effects of ARV drug exposure). Mothers should be advised not to breastfeed regardless of whether they are receiving ARV drugs for treatment of their HIV-1 disease. Parents and caregivers should be advised of the importance of prompt assessment if the infant becomes ill. For the infant in foster care, caregivers should have sufficient information about the infant's health, including HIV-1 exposure status, to ensure appropriate care.
Education should be provided regarding the lack of transmission risk in family activities such as eating, bathing, or sleeping together. The pediatrician has the opportunity to review prevention of HIV-1 transmission through safer sex practices, including encouraging condom use for all acts of sexual intercourse. Similarly, review of, or referral for, risk-reduction practices regarding injection drug use should be incorporated into visits when appropriate. Education and planning regarding future reproductive plans for the family, likely in collaboration with the family's adult HIV and gynecologic and obstetric providers, can minimize the risk of HIV-1 acquisition for sexual partners and MTCT in future pregnancies.
The necessity of maintaining confidentiality should be emphasized. There may be family members who are not aware of the mother's diagnosis, so caution should be exercised in the labor and delivery unit and when discussing the management of the infant in the postpartum unit. HIV-1 exposure and infection are not reasons for exclusion from infant child care or school. Pediatricians should discuss the need for planning for future care if the mother were to become ill with her HIV-1 infection.
HIV-1 Exposure and Infection Status Reporting
By the start of 2008, name-based HIV-1 reporting to state health departments is required in all states and territories for surveillance purposes. Many require reporting pregnancy in HIV-1–infected women and also require reporting the HIV-1 infection status of their infants. Collecting the maternal ARV treatment history, maternal demographics, labor and delivery record, and newborn records at the time of birth facilitates this required reporting. If reporting is delegated to another party, the pediatrician should facilitate the necessary information getting to the reporting provider.
Summary (see top)
Footnotes
All clinical reports from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.\
References
· Sanders GD, Bayoumi AM, Sundaram V, et al. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med. 2005;352 (6):570 –585[Abstract/Free Full Text]
· Immergluck LC, Cull WL, Schwartz A, Elstein AS. Cost-effectiveness of universal compared with voluntary screening for human immunodeficiency virus among pregnant women in Chicago. Pediatrics. 2000;105 (4). Available at: www.pediatrics.org/cgi/content/full/105/4/e54
· Gorsky RD, Farnham PG, Straus WL, et al. Preventing perinatal transmission of HIV: costs and effectiveness of a recommended intervention. Public Health Rep. 1996;111 (4):335 –341
· Centers for Disease Control and Prevention. Achievements in public health: reduction in perinatal transmission of HIV infection—United States, 1985–2005. MMWR Morb Mortal Wkly Rep. 2006;55 (21):592 –597[Medline]
· Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55 (RR-14):1 –17; quiz CE1–CE4[Medline]
· Perinatal HIV Guidelines Working Group. Public Health Service Task Force recommendations for use of antiretroviral drugs in pregnant HIV-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. Available at: http://aidsinfo.nih.gov/ContentFiles/PerinatalGL.pdf. Accessed July 2, 2008
· Havens PL, Mofenson LM; American Academy of Pediatrics, Committee on Pediatric AIDS. HIV testing and prophylaxis to prevent mother-to-child transmission in the United States. Pediatrics. 2008;122 (5):1127 –1134[Abstract/Free Full Text]
· King SM; American Academy of Pediatrics, Committee on Pediatric AIDS; Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Evaluation and treatment of the human immunodeficiency virus-1–exposed infant. Pediatrics. 2004;114 (2):497 –505[Abstract/Free Full Text]
· Connor EM, Sperling RS, Gelber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med. 1994;331 (18):1173 –1180[Abstract/Free Full Text]
· American College of Obstetricians and Gynecologists, Committee on Obstetric Practice. Prenatal and perinatal human immunodeficiency virus testing: expanded recommendations. ACOG Committee Opinion No. 304. Obstet Gynecol. 2004;104 (5 pt 1):1119 –1124[Medline]
· Fiscus SA, Schoenbach VJ, Wilfert C. Short courses of zidovudine and perinatal transmission of HIV [lett]. N Engl J Med. 1999;340 (13):1040 –1041; author reply 1042–1043[Free Full Text]
· Wade NA, Birkhead GS, Warren BL, et al. Abbreviated regimens of zidovudine prophylaxis and perinatal transmission of the human immunodeficiency virus. N Engl J Med. 1998;339 (20):1409 –1414[Abstract/Free Full Text]
· US Department of Health and Human Services, Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents. Rockville, MD: US Department of Health and Human Services; 2008. Available at: www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed July 2, 2008
· Wade NA, Zielinski MA, Butsashvili M, et al. Decline in perinatal HIV transmission in New York State (1997–2000). J Acquir Immune Defic Syndr. 2004;36 (5):1075 –1082[ISI][Medline]
· Capparelli EV, Mirochnick M, Dankner WM, et al. Pharmacokinetics and tolerance of zidovudine in preterm infants. J Pediatr. 2003;142 (1):47 –52[CrossRef][Medline]
· Working Group on Antiretroviral Therapy and Medical Management of HIV-Infected Children. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. Rockville, MD: US Department of Health and Human Services; 2008. Available at: http://aidsinfo.nih.gov/ContentFiles/PediatricGuidelines.pdf. Accessed July 2, 2008
· Dabis F, Bequet L, Ekouevi DK, et al. Field efficacy of zidovudine, lamivudine and single-dose nevirapine to prevent peripartum HIV transmission. AIDS. 2005;19 (3):309 –318[ISI][Medline]
· Lallemant M, Jourdain G, Le Coeur S, et al. Single-dose perinatal nevirapine plus standard zidovudine to prevent mother-to-child transmission of HIV-1 in Thailand. N Engl J Med. 2004;351 (3):217 –228[Abstract/Free Full Text]
· Taha TE, Kumwenda NI, Hoover DR, et al. Nevirapine and zidovudine at birth to reduce perinatal transmission of HIV in an African setting: a randomized controlled trial. JAMA. 2004;292 (2):202 –209[Abstract/Free Full Text]
· Eshleman SH, Hoover DR, Hudelson SE, et al. Development of nevirapine resistance in infants is reduced by use of infant-only single-dose nevirapine plus zidovudine postexposure prophylaxis for the prevention of mother-to-child transmission of HIV-1. J Infect Dis. 2006;193 (4):479 –481[CrossRef][ISI][Medline]
· Mirochnick M, Fenton T, Gagnier P, et al. Pharmacokinetics of nevirapine in human immunodeficiency virus type 1-infected pregnant women and their neonates. Pediatric AIDS Clinical Trials Group Protocol 250 Team. J Infect Dis. 1998;178 (2):368 –374[ISI][Medline]
· Musoke P, Guay LA, Bagenda D, et al. A phase I/II study of the safety and pharmacokinetics of nevirapine in HIV-1-infected pregnant Ugandan women and their neonates (HIVNET 006). AIDS. 1999;13 (4):479 –486[CrossRef][ISI][Medline]
· Tremoulet AH, Capparelli EV, Patel P, et al. Population pharmacokinetics of lamivudine in human immunodeficiency virus-exposed and -infected infants. Antimicrob Agents Chemother. 2007;51 (12):4297 –4302[Abstract/Free Full Text]
· Mandelbrot L, Landreau-Mascaro A, Rekacewicz C, et al. Lamivudine-zidovudine combination for prevention of maternal-infant transmission of HIV-1. JAMA. 2001;285 (16):2083 –2093[Abstract/Free Full Text]
· Moodley D, Moodley J, Coovadia H, et al. A multicenter randomized controlled trial of nevirapine versus a combination of zidovudine and lamivudine to reduce intrapartum and early postpartum mother-to-child transmission of human immunodeficiency virus type 1. J Infect Dis. 2003;187 (5):725 –735[CrossRef][ISI][Medline]
· Moodley D, Pillay K, Naidoo K, et al. Pharmacokinetics of zidovudine and lamivudine in neonates following coadministration of oral doses every 12 hours. J Clin Pharmacol. 2001;41 (7):732 –741[Abstract]
· Moodley J, Moodley D, Pillay K, et al. Pharmacokinetics and antiretroviral activity of lamivudine alone or when coadministered with zidovudine in human immunodeficiency virus type 1-infected pregnant women and their offspring. J Infect Dis. 1998;178 (5):1327 –1333[CrossRef][ISI][Medline]
· Persaud D, Palumbo P, Ziemniak C, et al. Early archiving and predominance of nonnucleoside reverse transcriptase inhibitor-resistant HIV-1 among recently infected infants born in the United States. J Infect Dis. 2007;195 (10):1402 –1410[Medline]
· Van Rompay KK, Otsyula MG, Marthas ML, et al. Immediate zidovudine treatment protects simian immunodeficiency virus-infected newborn macaques against rapid onset of AIDS. Antimicrob Agents Chemother. 1995;39 (1):125 –131[Abstract]
· Tsai CC, Follis KE, Sabo A, et al. Prevention of SIV infection in macaques by (R)-9-(2-phosphonylmethoxypropyl)adenine [lett]. Science. 1995;270 (5239):1197 –1199[Abstract/Free Full Text]
· Böttiger D, Johansson NG, Samuelsson B, et al. Prevention of simian immunodeficiency virus, SIVsm, or HIV-2 infection in cynomolgus monkeys by pre- and postexposure administration of BEA-005. AIDS. 1997;11 (2):157 –162[CrossRef][ISI][Medline]
· Dunn DT, Brandt CD, Krivine A, et al. The sensitivity of HIV-1 DNA polymerase chain reaction in the neonatal period and the relative contributions of intra-uterine and intra-partum transmission. AIDS. 1995;9 (9):F7 –F11[ISI][Medline]
· Read JS; American Academy of Pediatrics, Committee on Pediatric AIDS. Human milk, breastfeeding, and transmission of human immunodeficiency virus type 1 in the United States. Pediatrics. 2003;112 (5):1196 –1205[Abstract/Free Full Text]
· Shapiro RL, Ndung'u T, Lockman S, et al. Highly active antiretroviral therapy started during pregnancy or postpartum suppresses HIV-1 RNA, but not DNA, in breast milk [lett]. J Infect Dis. 2005;192 (5):713 –719[Medline]
· Palombi L, Marazzi MC, Voetberg A, Magid NA. Treatment acceleration program and the experience of the DREAM program in prevention of mother-to-child transmission of HIV. AIDS. 2007;21 (suppl 4):S65 –S71[CrossRef]
· Shapiro RL, Holland DT, Capparelli E, et al. Antiretroviral concentrations in breast-feeding infants of women in Botswana receiving antiretroviral treatment. J Infect Dis. 2005;192 (5):720 –727[CrossRef][ISI][Medline]
· Centers for Disease Control and Prevention. Guidelines for the prevention and treatment of opportunistic infections among HIV-exposed and HIV-infected children: recommendations from the Centers for Disease Control and Prevention, the HIV Medicine Association of the National Institutes of Health, Infectious Disease Society of America. MMWR Recomm Rep. 2008; In press. Available at: http://aidsinfo.nih.gov/contentfiles/Pediatric_OI.pdf. Accessed November 18, 2008
· Nesheim S, Palumbo P, Sullivan K, et al. Quantitative RNA testing for diagnosis of HIV-infected infants. J Acquir Immune Defic Syndr. 2003;32 (2):192 –195[ISI][Medline]
· Lambert JS, Harris DR, Stiehm ER, et al. Performance characteristics of HIV-1 culture and HIV-1 DNA and RNA amplification assays for early diagnosis of perinatal HIV-1 infection. J Acquir Immune Defic Syndr. 2003;34 (5):512 –519[CrossRef][Medline]
· Delamare C, Burgard M, Mayaux MJ, et al. HIV-1 RNA detection in plasma for the diagnosis of infection in neonates. The French Pediatric HIV Infection Study Group. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15 (2):121 –125[ISI][Medline]
· Read JS; American Academy of Pediatrics, Committee on Pediatric AIDS. Diagnosis of HIV-1 infection in children younger than 18 months in the United States. Pediatrics. 2007;120 (6). Available at: www.pediatrics.org/cgi/content/full/120/6/e1547
· Rouet F, Montcho C, Rouzioux C, et al. Early diagnosis of paediatric HIV-1 infection among African breast-fed children using a quantitative plasma HIV RNA assay. AIDS. 2001;15 (14):1849 –1856[CrossRef][ISI][Medline]
· Cunningham CK, Charbonneau TT, Song K, et al. Comparison of human immunodeficiency virus 1 DNA polymerase chain reaction and qualitative and quantitative RNA polymerase chain reaction in human immunodeficiency virus 1-exposed infants. Pediatr Infect Dis J. 1999;18 (1):30 –35[Medline]
· Karchava M, Pulver W, Smith L, et al. Prevalence of drug-resistance mutations and non-subtype B strains among HIV-infected infants from New York state. J Acquir Immune Defic Syndr. 2006;42 (5):614 –619[CrossRef][ISI][Medline]
· Geretti AM. HIV-1 subtypes: epidemiology and significance for HIV management. Curr Opin Infect Dis. 2006;19 (1):1 –7[ISI][Medline]
· Kline NE, Schwarzwald H, Kline MW. False negative DNA polymerase chain reaction in an infant with subtype C human immunodeficiency virus 1 infection [lett]. Pediatr Infect Dis J. 2002;21 (9):885 –886[CrossRef][ISI][Medline]
· Obaro SK, Losikoff P, Harwell J, Pugatch D. Failure of serial human immunodeficiency virus type 1 DNA polymerase chain reactions to identify human immunodeficiency virus type 1 clade A/G. Pediatr Infect Dis J. 2005;24 (2):183 –184[CrossRef][ISI][Medline]
· O'Donovan D, Ariyoshi K, Milligan P. Maternal plasma viral RNA levels determine marked differences in mother-to-child transmission rates of HIV-1 and HIV-2 in the Gambia. MRC/Gambia Government/University College London Medical School Working Group on Mother-Child Transmission of HIV. AIDS. 2000;14 (4):441 –448[CrossRef][ISI][Medline]
· Bremer JW, Lew JF, Cooper E, et al. Diagnosis of infection with human immunodeficiency virus type 1 by a DNA polymerase chain reaction assay among infants enrolled in the Women and Infants' Transmission Study. J Pediatr. 1996;129 (2):198 –207[CrossRef][ISI][Medline]
· Luzuriaga K, Sullivan JL. DNA polymerase chain reaction for the diagnosis of vertical HIV infection. JAMA. 1996;275 (17):1360 –1361[CrossRef][ISI][Medline]
· Centers for Disease Control and Prevention. Revised Surveillance Case Definitions for HIV Infection Among Adults, Adolescents, and Children Aged <18 Months and for HIV Infection and AIDS Among Children Aged 18 Months to <13 Years–United States, 2008. MMWR Morb Mortal Wkly Rep. 2008;57 (RR-10, December 5, 2008):1 –16[Medline]
· Dunn D; HIV Paediatric Prognostic Markers Collaborative Study Group. Short-term risk of disease progression in HIV-1-infected children receiving no antiretroviral therapy or zidovudine monotherapy: a meta-analysis. Lancet. 2003;362 (9396):1605 –1611[CrossRef][ISI][Medline]
· Moodley D, Bobat RA, Coutsoudis A, Coovadia HM. Predicting perinatal human immunodeficiency virus infection by antibody patterns. Pediatr Infect Dis J. 1995;14 (10):850 –852[ISI][Medline]
· Guar AH, Dominguez KL, Kalish ML, Rivera-Hernandez D, Donohoe M, Mitchell CD. Practice of offering a child pre-masticated (pre-chewed) food: an unrecognized possible risk factor for HIV transmission. Presented at: 15th Conference on Retroviruses and Opportunistic Infections: February 3–6, 2008; Boston, MA. Abstract 613b
· Simonds RJ, Oxtoby MJ, Caldwell MB, Gwinn ML, Rogers MF. Pneumocystis carinii pneumonia among US children with perinatally acquired HIV infection. JAMA. 1993;270 (4):470 –473[Abstract]
· Gibb DM, Davison CF, Holland FJ, Walters S, Novelli V, Mok J. Pneumocystis carinii pneumonia in vertically acquired HIV infection in the British Isles. Arch Dis Child. 1994;70 (3):241 –244[Abstract/Free Full Text]
· American Academy of Pediatrics. Tuberculosis. In: Pickering LK, Baker CJ, Long SS, McMillan JA, eds. Red Book: 2006 Report of the Committee on Infectious Diseases. Elk Grove Village, IL: American Academy of Pediatrics. 2006:678 –698
· Pacheco SE, McIntosh K, Lu M, et al. Effect of perinatal antiretroviral drug exposure on hematologic values in HIV-uninfected children: an analysis of the Women and Infants Transmission Study. J Infect Dis. 2006;194 (8):1089 –1097[CrossRef][ISI][Medline]
· Bunders MJ, Bekker V, Scherpbier HJ, Boer K, Godfried M, Kuijpers TW. Haematological parameters of HIV-1-uninfected infants born to HIV-1-infected mothers. Acta Paediatr. 2005;94 (11):1571 –1577[CrossRef][Medline]
· Feiterna-Sperling C, Weizsaecker K, Buhrer C, et al. Hematologic effects of maternal antiretroviral therapy and transmission prophylaxis in HIV-1-exposed uninfected newborn infants. J Acquir Immune Defic Syndr. 2007;45 (1):43 –51[CrossRef][Medline]
· Mofenson LM, Munderi P. Safety of antiretroviral prophylaxis of perinatal transmission for HIV-infected pregnant women and their infants. J Acquir Immune Defic Syndr. 2002;30 (2):200 –215[ISI][Medline]
· Thorne C, Newell ML. Safety of agents used to prevent mother-to-child transmission of HIV: is there any cause for concern? Drug Saf. 2007;30 (3):203 –213[Medline]
· Lambert JS, Nogueira SA, Abreu T, et al. A pilot study to evaluate the safety and feasibility of the administration of AZT/3TC fixed dose combination to HIV infected pregnant women and their infants in Rio de Janeiro, Brazil. Sex Transm Infect. 2003;79 (6):448 –452[Medline]
· Noguera A, Fortuny C, Munoz-Almagro C, et al. Hyperlactatemia in human immunodeficiency virus-uninfected infants who are exposed to antiretrovirals. Pediatrics. 2004;114 (5). Available at: www.pediatrics.org/cgi/content/full/114/5/e598
· Ekouevi DK, Touré R, Becquet R, et al. Serum lactate levels in infants exposed peripartum to antiretroviral agents to prevent mother-to-child transmission of HIV: Agence Nationale de Recherches Sur le SIDA et les Hepatites Virales 1209 study, Abidjan, Ivory Coast. Pediatrics. 2006;118 (4). Available at: www.pediatrics.org/cgi/content/full/118/4/e1071
· Alimenti A, Burdge DR, Ogilvie GS, Money DM, Forbes JC. Lactic acidemia in human immunodeficiency virus-uninfected infants exposed to perinatal antiretroviral therapy. Pediatr Infect Dis J. 2003;22 (9):782 –789[ISI][Medline]
· Dominguez K, Bertolli J, Fowler M, et al. Lack of definitive severe mitochondrial signs and symptoms among deceased HIV-uninfected and HIV-indeterminate children < or = 5 years of age, Pediatric Spectrum of HIV Disease project (PSD), USA. Ann N Y Acad Sci. 2000;918 :236 –246[ISI][Medline]
· Poirier MC, Divi RL, Al-Harthi L, et al. Long-term mitochondrial toxicity in HIV-uninfected infants born to HIV-infected mothers. J Acquir Immune Defic Syndr. 2003;33 (2):175 –183[ISI][Medline]
· Blanche S, Tardieu M, Rustin P, et al. Persistent mitochondrial dysfunction and perinatal exposure to antiretroviral nucleoside analogues. Lancet. 1999;354 (9184):1084 –1089[CrossRef][ISI][Medline]
· European Collaborative Study. Exposure to antiretroviral therapy in utero or early life: the health of uninfected children born to HIV-infected women. J Acquir Immune Defic Syndr. 2003;32 (4):380 –387[ISI][Medline]
· Spector SA, Saitoh A, Spector SA, Saitoh A. Mitochondrial dysfunction: prevention of HIV-1 mother-to-infant transmission outweighs fear [lett]. AIDS. 2006;20 (13):1777 –1778[Medline]
· Blanche S, Tardieu M, Benhammou V, et al. Mitochondrial dysfunction following perinatal exposure to nucleoside analogues. AIDS. 2006;20 (13):1685 –1690[Medline]
· Barret B, Tardieu M, Rustin P, et al. Persistent mitochondrial dysfunction in HIV-1-exposed but uninfected infants: clinical screening in a large prospective cohort. AIDS. 2003;17 (12):1769 –1785[CrossRef][ISI][Medline]
· Brogly SB, Ylitalo N, Mofenson LM, et al. In utero nucleoside reverse transcriptase inhibitor exposure and signs of possible mitochondrial dysfunction in HIV-uninfected children. AIDS. 2007;21 (8):929 –938[ISI][Medline]
· Warszawski J, Lechenadec J, Faye A, et al. Long-term nonprogression of HIV infection in children: evaluation of the ANRS prospective French Pediatric Cohort. Clin Infect Dis. 2007;45 (6):785 –794[Medline]
· Ofori-Mante JA, Kaul A, Rigaud M, et al. Natural history of HIV infected pediatric long-term or slow progressor population after the first decade of life. Pediatr Infect Dis J. 2007;26 (3):217 –220[Medline]
· Guay LA, Musoke P, Fleming T, et al. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancet. 1999;354 (9181):795 –802[ISI][Medline]
· Boucher FD, Modlin JF, Weller S, et al. Phase I evaluation of zidovudine administered to infants exposed at birth to the human immunodeficiency virus. J Pediatr. 1993;122 (1):137 –144[ISI][Medline]